Blood
Normally, the concentration of red blood cells in urine is very low (0-5 erythrocytes/µL). This concentration is below the detection limit of the test strips.
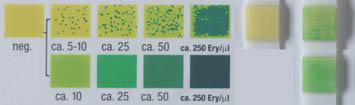
Test strip, from left to right: comparison scale, the upper row showing the reaction with intact erythrocytes, the lower row showing the reaction with lysed erythrocytes. Then there is a negative result, and 2 positive results for each type of reaction.
Hematuria
Hematuria refers to the presence of red blood cells in urine, which is pathological in most cases.
Macrohematuria
The urine is red and contains blood that is visible from a concentration of 0.5 µL of blood per liter of urine
Microhematuria
The urine has a typical color. However, a red stain is visible after centrifugation at the bottom of the tube. Microhematuria is defined by a concentration of more than 5-10 erythrocytes/µL measured by the test strip. With the microscopic examination of urinary sediment, microhematuria is defined by observing 5-10 erythrocytes by HPF (HPF = High Power Field) with a 400x magnification.
Hematuria detected chemically by the test strip should always be examined microscopically in the sediment. A red color due to substances other than blood is described in the "Color" section of the chapter "Testing the physical properties".
Clinical relevance
Hematuria is often detected by the test strips. Most hematuria originate in the uro-genital tract
Pre-renal hematuria :
Hemorrhagic diathesis, hemophilia, thrombopathies, anticoagulant therapy, physical stress (sport) hematuria.
Renal hematuria:
Glomerulonephritis (often presents with a combination with erythrocyte casts and proteinuria), lupus erythematosus, periarteritis nodosa, polycystic kidney, diabetic nephropathy or gout, pyelonephritis, renal tumors, and microcrystaluria (i.e. uric acid, calcium).
Post-renal hematuria:
Urolithiasis, kidney and urinary tract trauma or tumor
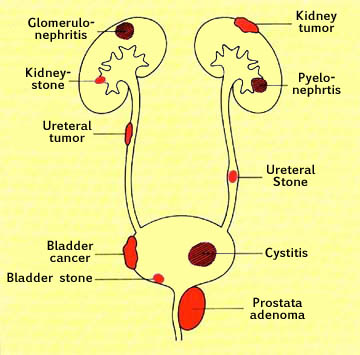
Renal and post-renal causes of hematuria
Hemoglobinuria
Hemoglobinuria occurs during intravascular hemolysis. Hemoglobin appears in urine when the binding capacity of haptoglobin in plasma and tubular reabsorption capacity is saturated. This is usually the case for plasma hemoglobin concentrations above 60 µmol/L.
The main causes of hemomoglobinuria are:
- Hematuria (lysis of erythrocytes)
- Genetic forms of congenital hemoglobinuria
- congenital hemolytic anemia
- Acquired forms of hemolytic anemia
- transfusion reaction
- Burns
- Bacterial hemolysins (streptococcal infection), sepsis
- Degradation of red blood cells (freezing, walking, hemolytic anemia of microangiopathy)
- Paroxysmal nocturnal hemoglobinuria PNH
Myoglobinuria
Myoglobin is a muscle molecule that appears in urine in case of muscle damage.
The main causes of myoglobinuria are:
- Muscle necrosis
- "Crush"-Syndrom (concussion and multiple contusions)
- Arterial ischemia of the extremities, myocardial infarction
- Surgery
- Metabolische Myoglobinurie
- Metabolic myoglobinuria hereditary myopathy (i.e. MacArdle disease)
- Malignant hyperthermia
- Carnitin-palmityl-transferase deificency
- Intense muscular effort
- Toxic Substance
- Haff disease
- Snake bite
- Drugs
- Autoimmune diseases
- Polymyositis
Specidicity
The test is specific for hemoglobin and myoglobin, but it can not differentiate the two substances. It is not influenced by other cellular components of urine.
On some test strips, there are different scales for the colorimetric determination of erythrocytes and hemoglobin.
.
Note: lysed erythrocytes give a positive reaction but are not visible under a microscope. Intact erythrocytes produce a dotted colored reaction while lysed erythrocytes produce diffuse coloration of the reactive zone.

Test strip, from left to right: negative result, then erythrocyturia, then hemoglobinuria.